Introduction
Nyctophobia symptoms can severely impact a person’s mental well-being, making daily life and sleep difficult. Nyctophobia, commonly known as an intense fear of darkness, is more than just discomfort—it is a specific phobia that triggers anxiety and distress. While some fear of the dark is natural, severe nyctophobia symptoms can interfere with routine activities, emotional stability, and overall health.
In this article, we will explore seven common nyctophobia symptoms, their effects, and when to seek help.

If you need professional support, consulting the best psychiatrist in Delhi can provide valuable insights and personalized strategies for Phobias. Consider Visiting:
1. Extreme Anxiety in Darkness
One of the most common nyctophobia symptoms is overwhelming anxiety when exposed to darkness. People may experience an increased heart rate, dizziness, sweating, or even a panic attack when they find themselves in a dark environment.
2. Avoidance of Dark Places
Individuals with nyctophobia symptoms tend to avoid situations where they might be in darkness. This could mean refusing to enter dimly lit rooms, avoiding nighttime travel, or keeping lights on even when unnecessary.
3. Difficulty Sleeping Due to Fear of Darkness
People with nyctophobia symptoms often struggle to sleep in complete darkness. They may insist on sleeping with multiple lights on, experience frequent awakenings at night, or have trouble falling asleep due to anxiety.
4. Physical Reactions to Darkness
Nyctophobia is not just a mental condition—it also triggers physical symptoms, including:
- Rapid heartbeat
- Sweating
- Trembling
- Shortness of breath
- Nausea or dizziness
These reactions occur due to the body’s fight-or-flight response, perceiving darkness as a threat.
5. Disturbing Thoughts and Nightmares
Another key nyctophobia symptom is the presence of distressing thoughts or nightmares related to darkness. The individual may fear imaginary threats, supernatural elements, or past traumatic events associated with the dark.
6. Emotional Distress and Mood Swings
Persistent fear of darkness can lead to mood swings, irritability, and emotional instability. Individuals with severe nyctophobia symptoms may feel embarrassed discussing their fear, leading to social withdrawal or isolation.
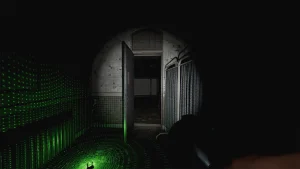
7. Overdependence on Light Sources
People with nyctophobia symptoms may develop an extreme reliance on light sources to feel safe. They may refuse to stay in dimly lit areas, keep flashlights nearby, or even experience distress when facing sudden power cuts.
When to Seek Professional Help
While mild fear of darkness is common, severe nyctophobia symptoms require professional intervention. Therapy, relaxation techniques, and cognitive behavioral therapy (CBT) can help manage and overcome this phobia.
The Role of Therapy and Treatment in Managing Nyctophobia
Overcoming nyctophobia symptoms often requires a combination of therapeutic approaches and lifestyle changes. Many individuals benefit from cognitive behavioral therapy (CBT), which helps identify and reframe negative thought patterns associated with darkness. Exposure therapy is another effective method, where individuals are gradually introduced to dim lighting in a controlled environment to reduce fear responses over time.
For more information on phobias and mental health, refer to these authoritative sources:

Conclusion
Recognizing nyctophobia symptoms is the first step toward overcoming the fear of darkness. If this phobia affects daily life, professional help can provide effective treatment strategies. With the right support, individuals can regain control over their fears and improve their overall well-being.
With the right combination of therapy, gradual exposure, and support from professionals, individuals can regain confidence and learn to manage their fears effectively. Seeking help is not a sign of weakness but a proactive step toward better mental health.
If you or someone you know struggles with nyctophobia symptoms, reaching out to a qualified therapist can make a significant difference. Professional guidance, coupled with self-help strategies, can lead to long-term improvement and a better quality of life.